Physical Therapy Videos - Hip and Pelvis
What Is It?
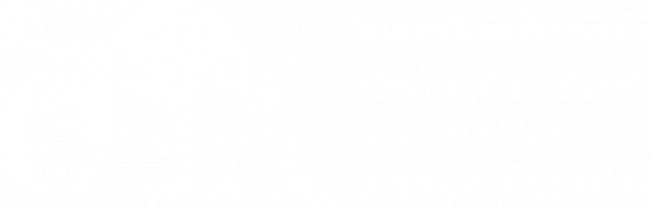
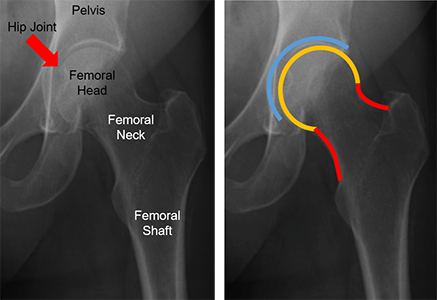
The human hip joint is like a ball and socket. The top part of the thigh bone (femur) is the ball, and it fits into the hip socket. The thigh bone has a part called the femoral neck that connects the ball to the long part of the bone. The hip has big muscles around it that help you move your leg. The blood vessels and nerves for your hip and leg are in the front and back.
How It Happens
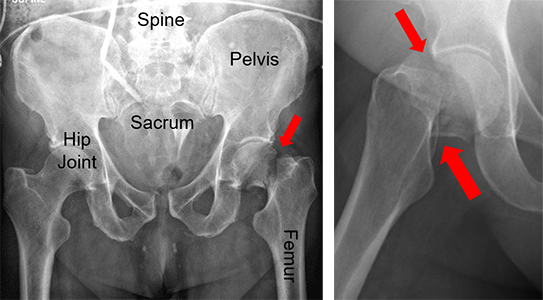
Broken hips are common in people over 65 because bones get weaker as we age. These breaks usually happen when someone falls on their hip. Broken hips can also happen from car accidents or jumping off something like a ladder.
First Steps
Broken hips hurt a lot and make it hard or impossible to walk. People with broken hips usually go to the emergency room. At the hospital, doctors take X-rays and give pain medicine. Most broken hips need surgery and a stay in the hospital. Before surgery, doctors check your health and may do more tests.
Treatment
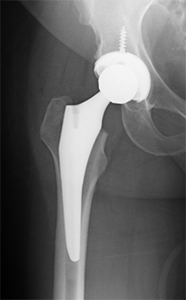
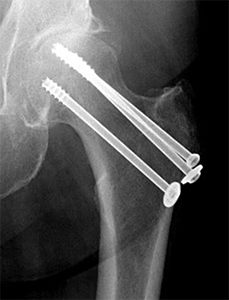
Surgery is the main way to treat a broken hip. Doctors can fix the break with screws, a plate, or replace part or all of the hip joint. Some broken hips need a partial or total hip replacement. Your surgeon will talk to you about which option is best for you. Surgery usually happens within 48 hours of the injury. If you are too sick, surgery may need to be delayed longer.
Recovery
After surgery, patients do physical therapy to get stronger and walk normally again. It's important to get moving as soon as possible to avoid problems like bed sores, blood clots, and pneumonia. You may need to go to a rehab center before going home. Always follow your surgeon's instructions.
Long Term
After surgery, patients might need a walker or cane for a while. It's important to prevent future falls and talk to your doctor about your bone health. Problems like blood clots, infections, and limping can happen, but they're not common. Some patients might need more surgery for certain complications or if the bone doesn’t heal.
Physical Therapy Videos - Hip and Pelvis
More Information
---
Nicholas M. Romeo, DO
Edited by the OTA Patient Education Committee and Justin Haller, MD (section lead)
All x-rays and pictures taken from the personal collection of Dr. Romeo and Christopher Domes, MD