Physical Therapy Videos - Foot & Ankle
What Is It?
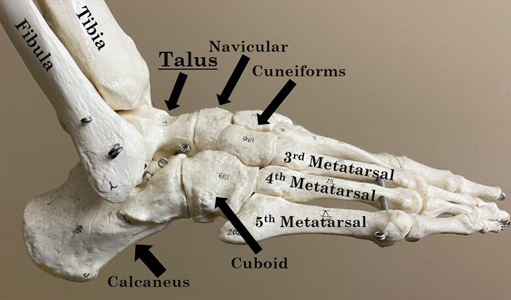
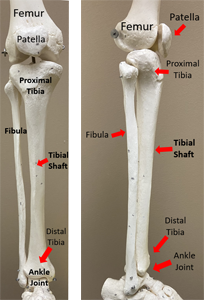
The ankle has three bones: the tibia (shin bone), the fibula (smaller leg bone) and the talus. These bones work together to let the ankle move. Ligaments connect the bones together. There are nerves and blood vessels on the front of the ankle as well and the inside and outside.
How It Happens
Ankle fractures are common. They usually happen from a twist and fall, like on wet floors, grassy hills, stairs, or curbs. Since there are many bones and ligaments, one or many of these structures can be hurt. The most common break is in the fibula (smaller leg bone).
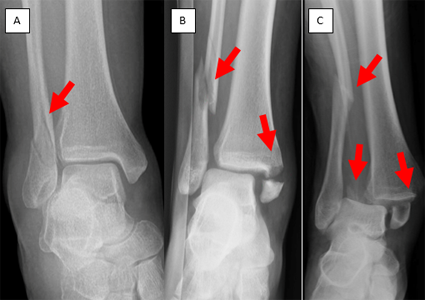
Types of Ankle Fractures
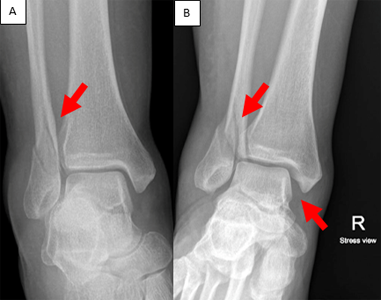
The more serious the injury, the more likely it will need surgery. Ankle fractures can have one, two, or three broken bones. When two bones are broken, it's called a bimalleolar ankle fracture. When three bones are broken, it's called a trimalleolar ankle fracture. Stable fractures can sometimes heal with a cast or boot. Unstable fractures may need surgery. Unstable ankle fracture mean the talus bone moves and the tibia and fibula can't keep it in place.
First Steps
Ankle fractures are usually very painful. In the emergency room, the doctor will check your foot, ankle, and take x-rays. They might put a splint or boot on your ankle. If your ankle is out of place, the doctor will put it back in place and apply a splint or boot. If surgery is needed, it's usually done within five to ten days, but might be delayed if your ankle is swollen.
Treatment
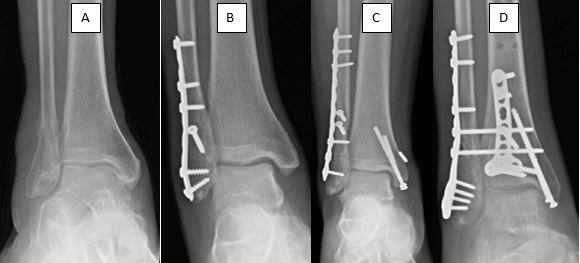
Some ankle fractures can be treated with a protective boot and early weight-bearing. More serious injuries may need surgery. Surgery helps the ankle heal and allows for early movement to avoid stiffness. Your doctor will decide the best timing and method for surgery.
Recovery
After surgery, you'll wear a plaster splint or a boot to protect your ankle. To reduce swelling, keep your foot elevated and avoid putting weight on it. You'll see your surgical team about one to two weeks after surgery to check on your healing. You might start doing home exercises or even start putting some weight on it. You may need physical therapy to help with movement and weight bearing.
Long Term
Most simple ankle fractures heal well, but more serious injuries might cause long-term issues. These include stiffness, soreness, and pain. You may need several months of physical therapy to return to your normal activities. Your injured ankle may always feel different from your uninjured ankle. Some people may develop arthritis after an ankle fracture, which can cause pain and stiffness. Your doctor can discuss treatment options with you if this happens. The plates and screws may bother you. If the bones have healed you can talk to your surgeon about having them removed.
Physical Therapy Videos - Foot & Ankle
More Information
Adults:
Children:
---
Babar Shafiq, MD
Edited by the OTA Patient Education Committee
All x-rays and pictures taken from the personal collections of Dr. Shafiq and Christopher Domes, MD