Session IX - Tibia
Anatomic and Biomechanical Considerations Using a Lateral Starting Approach for Intramedullary Nailing of Proximal Third Tibia Fractures
Ronald Wobig, MD; Sean W. McLoughlin, PhD; Pramod Maheshwari, BS; James Green; Paul J. Duwelius, MD, Oregon Health Sciences University, Portland, OR
Purpose: Intramedullary fixation of tibia fractures is a standard of treatment. Biomechanical fixation, preservation of soft tissue structures, and technical advantages have made this the preference when dealing with acute fracture management. However, it has also been shown that proximal third tibia fractures are a difficult entity to manage due to malreduction (Freedman E.; Clin Orthop 315:25-33;1995, Henley MB; J Orthop Trauma 7:311-19;1995). Anterior displacement and excessive valgus deformity are commonly encountered abnormalities seen with fracture management of proximal third tibia fractures. The purpose of this study was to determine if a lateral versus a "traditional" medial starting point would maximize anatomical considerations and biomechanical insertion characteristics.
Methods: Eleven matched pairs of fresh frozen cadaver lower extremities were obtained and examined for fracture, surgery, pathologic lesions and/or osteopenia. Each specimen was potted in plaster at its distal aspect and affixed with two 3-element 45E rosette strain gauges (Micromeasurements Group, Raleigh, N.C.). One rosette was placed on the tibial tubercle, at 5 cm below the tibial plateau, and the second rosette was placed in the same orientation on the posterior cortex. Half of the specimens had a medial starting point made at the intersection of the anterior metaphyseal cortex and the medial tibia eminence. The other half of the matched pairs had a lateral starting point made at the intersection of the anterior metaphysical cortex and the lateral tibial eminence. In the sagital plane, both starting points were made as close to the anterior tibial cortex as possible while still remaining within the intramedullary canal. All insertion sites were made by the same surgeon using a canulated cutter. An unreamed AO tibial nail (Synthes, Paoli,PA) was held in a MTS minibionix servohydraulic testing machine (MTS Systems, Prairie Eden, MN) using a specially designed fixture. The nail was inserted at a fixed rate of 1 mm/sec, while collecting force, axial torque, displacement and strain.
To determine the potential for anterior displacement, angulation and rotational deformities with tibial IM nailing, a second test was performed on the matched tibial pairs. A "fracture" was created by using a reciprocating saw at approximately 6 cm distal to the tibial plateau in the horizontal plane. A Polhemus (Polhemus Inc., Cochester, VT) electromagnetic tracker was used to determine displacement, angulation and rotational changes of the proximal fragment in reference to the distal shaft.
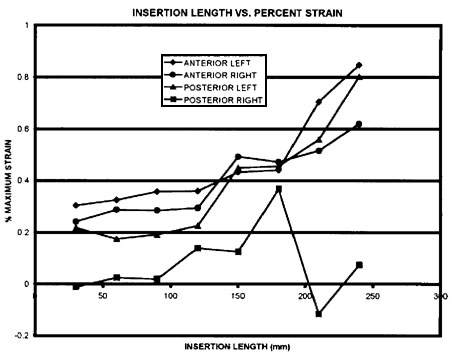
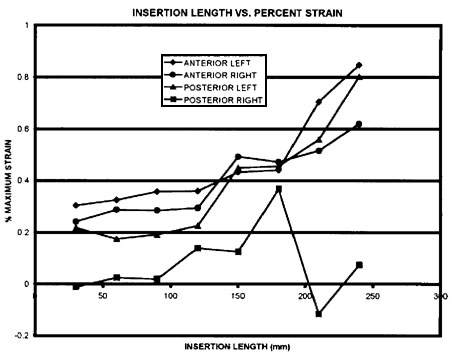
Results: Maximum principal strain (s1) values for anterior and posterior rosette gages are presented in Figure 1. Data are presented as a percent of the pairwise maximum value observed throughout the test. The strains observed on the anterior aspect of the tibia were lower for the medial approach at each point measured until 210mm, when the strain in the lateral approach specimens exceeded the medial approach specimen. An analysis of variance (ANOVA) did not find the anterior strains to be significantly different (p<0.05). Strain in the posterior rosette was uniformly greater in the medial approach specimens. An ANOVA indicated that the posterior strains were significantly higher in the medial approach specimens (p<0.05). Insertion force data are presented in Figure 2. Compressive force is also presented as a pairwise maximum percent of force throughout the insertion process. Force was greater for the medial specimens until the 240mm point
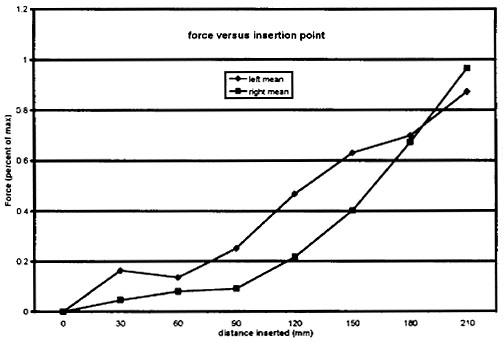
where lateral force slightly exceeded force in the medial specimens. An ANOVA showed the medial specimens to have statistically higher force (P<0.05). Axial torque also was shown to be statistically greater in the medial approach specimens as compared to the lateral approach (P<0.05) (data not shown). Preliminary testing indicates a trend for higher anterior displacement of the proximal fragment in the medial approach specimens.
Discussion: Malalignment of proximal third tibia fractures has been recognized to be due in part to the force generated by the patellar tendon and local soft tissues acting to translate the proximal tibia anteriorly (Fanre C; Transition des Membres, p102;1987). In addition, a medial starting point contributes to increased force and fracture displacement. Anatomical studies in our lab have shown that the proximal tibia has a larger sagital dimension laterally as compared to medially. This is best visualized as the proximal tibia being in the shape of a triangle. The medial aspect is at the apex, and the lateral aspect is at the base of the triangle. The proximal anterior cortex also has a steeper anterior-posterior slope medially when compared to the lateral slope. Alms demonstrated that the intramedullary canal exits on the margin of the lateral articular facet when placing a drill from the plafond to the tibial plateau. Measurements of strain, torque and force in this study has supported our assumption that a lateral starting point would diminish these parameters acting to cause malreduction in tibial nailing. This would eliminate the need for external fixation, unicortical buttress plating or the placement of physical reduction maneuvers to hold the proximal fracture piece reduced while IM nailing. However, certain fractures could still be difficult to reduce even with these recommendations and must be treated on a individual basis. Fracture reduction and ease of tibial intramedullary fixation is based upon the neutralization of the primary factors causing malreduction. We have shown that neutralization of the insertion site can be accomplished by approaching tibial intramedullary nailing through a lateral approach.
Conclusion: Our study has shown that a lateral starting point utilizes anatomical considerations to minimize deforming biomechanical forces for tibial IM nailing. By taking advantage of the lateral approach, one should be able to minimize anterior displacement, valgus angulation and rotational deformities when dealing with proximal third tibia fractures. In addition, we would also suggest that a lateral approach could be used for all fractures of the tibia to be managed with rigid intramedullary fixation. Further implications include nail construction (stiffness and cross-sectional shape), with evaluation of lessening the angle of the proximal bend, to further decrease biomechanical forces generated. Further investigation will be necessary to fully evaluate such changes.