Session VII - Foot / Ankle
Sat., 10/12/13 Foot/Ankle, PAPER #82, 10:52 am OTA 2013
The Fate of the Fixed Syndesmosis Over Time
Scott Koenig, MD; Elisabeth Gennis, MD; Deirdre Rodericks, BS; Peters Otlans, BS;
Paul Tornetta, III, MD;
Boston University Medical Center, Boston, Massachusetts, USA
Background/Purpose: A prior study demonstrated statistical widening of the syndesmosis within weeks of elective screw removal. However, no information is available as to the radiographic outcomes of screw retention. The purpose of this study is to evaluate syndesmotic widening and talar shift over time in patients treated with syndesmotic screws and to compare removal versus retention along with other potential risk factors that may lead to syndesmotic widening over time.
Methods: A consecutive series of patients with ankle fractures and associated syndesmotic disruption treated with open reduction and internal fixation (ORIF) were reviewed. Demographic data, fracture classification, fixation, syndesmotic screw outcomes (removal, loosening/breakage, or retained and solid), and radiographic findings (MCS = medial clear space, CS = tibia-fibula space, and OL =tibia-fibula overlap) on the mortise and AP radiographs were evaluated at presentation, immediately postoperative, and final follow-up at a median of 6 months. Screw removal was offered to patients and performed at 12 weeks if chosen. T tests were used to compare postoperative and final follow-up measurements as well as groups of interest.
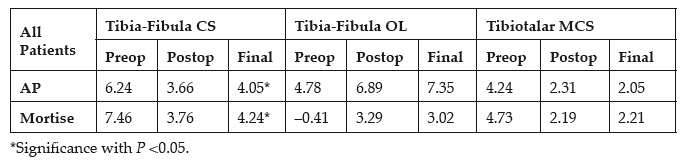
Results: 166 patients (94 men and 72 women) aged 16 to 83 years (average = 39.9) treated operatively for syndesmotic disruption comprise the study population. There were 84 SE (supination external rotation), 54 PE (pronation external rotation), and 28 PA (pronation abduction) injuries. 39 (23%) presented with dislocation. 123 were treated with a plate and syndesmotic screws and 43 with syndesmosis-only fixation. Postoperative radiographic alignment was not affected by fracture type, presence of initial dislocation, or use of a plate. 58 (35%) of the patients had their screws removed by choice, and at final follow-up 17 (16%) of the remaining patients’ screws were solid and 91 (84%) were loose or broken. The following table details the measurements for all patients:
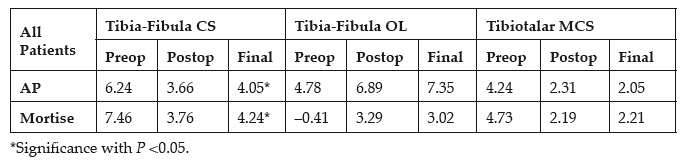
There was an approximately 0.5-mm shift in the fibula over time compared to the postoperative radiograph (AP, P =0.02; mortise, P = 0.003) without any change in MCS, indicating that the mortise remained intact without talar shift. We compared those whose screws were removed versus retained, screws removed grouped with those that were loose/broken versus solid and retained, those who presented dislocated versus not, fixed with a plate versus screws only, and Weber B versus C injuries on the AP and mortise views for all measurements. The only significant finding was a slightly greater CS (4.6 mm vs 4.1 mm, P = 0.02) and lower OL (2.4 mm vs 3.3 mm, P = 0.03) on the mortise view for those whose screws were removed by choice as compared with those whose screws were retained, regardless of loosening or breakage. These differences were only 0.5 mm and 1.1 mm, and did not reach statistical significance after adjusting for multiple evaluations (reset of P <0.005 Bonferroni correction).
Conclusion: In contradistinction to prior work, we found only very mild widening (0.5 mm) of the tibia-fibula space occurs over time after syndesmotic fixation. Removal of syndesmotic screws at 3 months results in slightly less OL (~ 1 mm) and greater CS (0.5 mm) than screw retention even if the retained screws loosened or broke, but this was not associated with any talar subluxation. These differences were not statistically significant, and were quite small (<1 mm). The mortise in patients remains intact regardless of whether the syndesmotic screws are removed, loosen or break, or remain solid and in place.
Alphabetical Disclosure Listing
• The FDA has not cleared this drug and/or medical device for the use described in this presentation (i.e., the drug or medical device is being discussed for an “off label” use). ◆FDA information not available at time of printing. Δ OTA Grant.