Session I - Polytrauma / Pelvis / Post-Traumatic Reconstruction
Thurs., 10/10/13 Polytrauma/Pelvis/Post-Trauma, PAPER #28, 3:20 pm OTA 2013
Time to Definitive Operative Treatment Following Open Fracture Does Not Impact Development of Deep Infection: A Prospective Cohort Study of 736 Subjects
Donald Weber, MD1; Sukhdeep K. Dulai, MD, MSc, FRCS(C)1; Joseph Bergman, MD1;
Richard E. Buckley, MD2; Lauren A. Beaupre1;
1University of Alberta, Edmonton, Alberta, Canada;
2University of Calgary, Calgary, Alberta, Canada
Purpose: The primary study objective was to evaluate the relationship between time to definitive orthopaedic surgical management and development of deep infection in open long bone fractures (humerus, radius/ulna, femur, tibia/fibula). Secondarily, we examined the association of Gustilo grade and fracture location with development of deep infection.
Methods: Between 2001 and 2008, 736 subjects with 791 open fractures were enrolled in a prospective cohort study undertaken at three Level I trauma centers. Demographics, injury information (Gustilo grade, fracture site), and time from injury to definitive surgical management were recorded. Subjects were evaluated at outpatient clinics using standardized data forms until the fracture healed. Phone interviews were undertaken at 1 year postfracture to confirm outcomes. Deep infection was defined as purulent drainage or osteomyelitis presenting after wound closure. Descriptive analyses were initially undertaken on time from injury to definitive surgical management calculated in hours, Gustilo grade, and fracture location (upper extremity, femur, tibia/fibula). Multivariate logistic regression was undertaken on time from injury to surgery, Gustilo grade and fracture location with deep infection (yes/no) as the dependent variable.
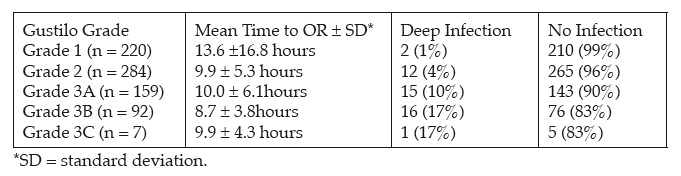
Results: Most subjects were male (n = 530 [72%]) and the mean age was 41.5 ± 17.1 years. Almost half (n = 359 [49%]) of injuries occurred in motor vehicle accidents; falls (n = 230 [31%]), crush injuries (n = 131 [18%]) and assaults (n=16 [2%]) were other mechanisms of injury. Tibial/fibular fractures were most common (n = 413 [52%]), followed by upper extremity (n = 285 [36%]) and femoral (n = 93 [12%]) fractures. Overall, 636 (86%) subjects (685 fractures) completed the 1-year interview; only 39 (5%) subjects (43 fractures) did not complete either clinic visits or the 1-year interview. Of 753 fractures with outcomes, 46 (6%) developed deep infections. The mean time to surgery was 10.9 ± 10.6 hours for those without and 8.7 ± 4.4 hours for those with deep infection (P = 0.17). Of those with infection, 9 (21%) underwent surgery within 6 hours, 28 (65%) between 6 and 12 hours, and 6 (14%) after 12 hours of injury. In general, time to operating room (OR) decreased as Gustilo grade increased (P <0.001) while infections increased with increasing Gustilo grade (P <0.001).
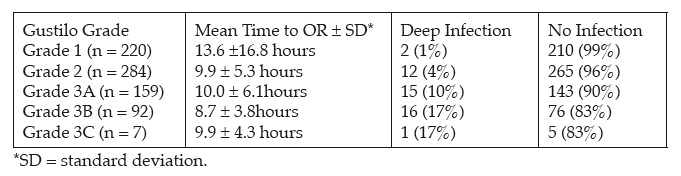
Four (1.5%) upper extremity, seven (8%) femoral, and 34 (9%) tibial/fibular fractures developed deep infections (P = 0.001). Multivariate logistic regression showed no significant association between developing deep infection and mean hours to operative management (odds ratio [OR] 0.97; 95% confidence intervals [95% CI] 0.90, 1.1) while Grades 3A (OR 6.6; 95%CI 1.5, 30.2) and 3B (OR 13.4; 95%CI 2.9, 61.9) relative to Grade 1 injuries and tibia/fibular (OR 4.0; 95%CI 1.4, 11.8) relative to upper extremity fractures were significantly associated with developing deep infection.
Conclusion: Development of deep infection after open fracture was not associated with time to surgery; instead increasing Gustilo grade or tibial/fibular fractures were associated with developing a deep infection. With the low number of infections seen in Grade 1 and 2, and all upper extremity open fractures, there may be clinical implications for determining if an open fracture requires surgery in the middle of the night, especially if a trauma room is available in the morning.
Alphabetical Disclosure Listing
• The FDA has not cleared this drug and/or medical device for the use described in this presentation (i.e., the drug or medical device is being discussed for an “off label” use). ◆FDA information not available at time of printing. Δ OTA Grant.