Sat., 10/6/12 Tibial Fractures, PAPER #118, 4:32 pm OTA-2012
Soft-Tissue Injury Predictors of Amputation Following Severe Open Tibia Fractures
MAJ Kenneth J. Nelson, MD1; LTC Anthony E. Johnson, MD2; Clifford B. Jones, MD3;
Renan C. Castillo, PhD4; Anthony R. Carlini, MS4; Michael J. Bosse, MD5;
Ellen J. MacKenzie, PhD4; for the LEAP (Lower Extremity Assessment Project) Study Group;
1William Beaumont Army Medical Center, El Paso, Texas, USA;
2Brooke Army Medical Center, San Antonio, Texas, USA;
3Orthopaedic Associates of Michigan, Michigan State University, Grand Rapids, Michigan, USA;
4Johns Hopkins Bloomberg School of Public Health, Baltimore, Maryland, USA;
5Carolinas Medical Center, Charlotte, North Carolina, USA
Purpose/Hypotheses: There is great clinical interest in identifying the type and extent of soft-tissue injuries that limit the ability to reconstruct injured limbs. Detailed soft-tissue injury data from a large prospective study of limb-threatening injuries may be used to identify the muscles, vessels, and nerves that contribute the most toward predicting amputation. The information gained may allow surgeons to better counsel patients and set their expectations after the initial débridement and to identify areas for future surgical research.
Methods: This was a secondary analysis of data from 347 patients with unilateral grade III tibia fractures from a prospective observational study at 8 Level I trauma centers. Of these, 265 patients were treated via salvage and 82 via amputation. Soft-tissue injuries for each of the 4 compartments in the tibia were classified by listing the contents of each compartment (11 muscles, 3 nerves, and 5 vessels) and grading them as 1 (no injury), 2 (impaired), or 3 (nonfunctional or absent). The main outcome measure for this analysis was amputation during the initial hospitalization. Separate hierarchical stepwise logistic regression modeling techniques were used to identify significant predictors of amputation. Results are reported as odds ratios (OR) with 95% confidence intervals (CI). In this abstract, we report all items with ORs indicative of a 300% or greater increase in the risk of amputation.
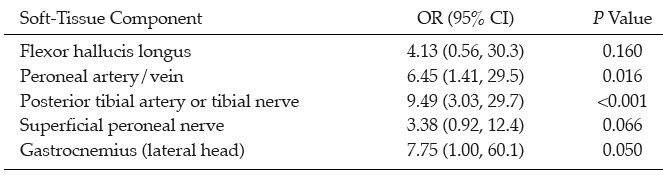
Results: Detailed soft-tissue injury data were strongly predictive of amputation. All 19 items were able to predict amputation with an area under the curve (AUC) of 0.833 (roughly equivalent to 80% sensitivity and specificity). Two components, the posterior tibial artery and the tibial nerve, were so highly correlated that it would have been impossible to include them as separate items in any model, and were merged for this analysis. Using logistic regression we identified a subset of six items (see table), which accounted for 98% of the predictive power of the larger model (AUC = 0.815).
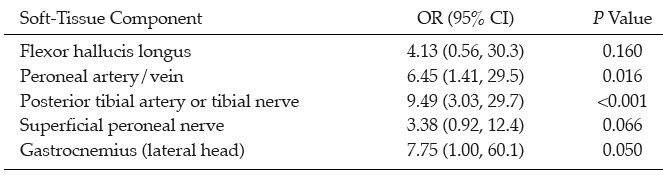
Conclusion: In a detailed analysis of the individual structures involved in a mangled lower extremity, specific muscle, vascular, and nerve injuries are strong predictors of amputation. Specifically, injury to the flexor hallucis longus and gastrocnemius (lateral head) muscles, the peroneal artery/vein, the posterior tibial artery, and the tibial and superficial peroneal nerves substantially increased the chances of amputation. It is also notable the extent to which these six components accounted for the predictive power of the complete detailed dataset. These results may allow surgeons to more accurately counsel their patients on what to expect and enable them to maximize the predicted functional outcome for a patient with a mangled lower extremity.
Alphabetical Disclosure Listing (808K PDF)
• The FDA has not cleared this drug and/or medical device for the use described in this presentation (i.e., the drug or medical device is being discussed for an “off label” use). ◆FDA information not available at time of printing. Δ OTA Grant.