Fri., 10/5/12 Basic Science, PAPER #54, 1:35 pm OTA-2012
Chitosan: An Effective NPWT-Compatible Local Antibiotic Delivery Device
Ben C.C. Rand, MRCS1,2; Scott P. Noel, PhD3; Joseph C. Wenke, PhD1;
1U.S. Army Institute of Surgical Research, Fort Sam Houston, Texas, USA
1,2Academic Department of Military Surgery and Trauma, Royal Centre for Defense Medicine, Birmingham, United Kingdom;
3Bionova Medical, Memphis, Tennessee, USA
Purpose: Antibiotic-loaded polymethylmethacrylate (PMMA) beads are not an ideal antibiotic vehicle, and negative pressure wound therapy (NPWT) has been shown to reduce their effectiveness. It appears that negative pressure removes the eluted antibiotic from the wound before it can diffuse throughout the wound. We hypothesized that antibiotic-impregnated chitosan sponges would effectively reduce bacteria when used with NPWT due to its increased contact with the wound surface.
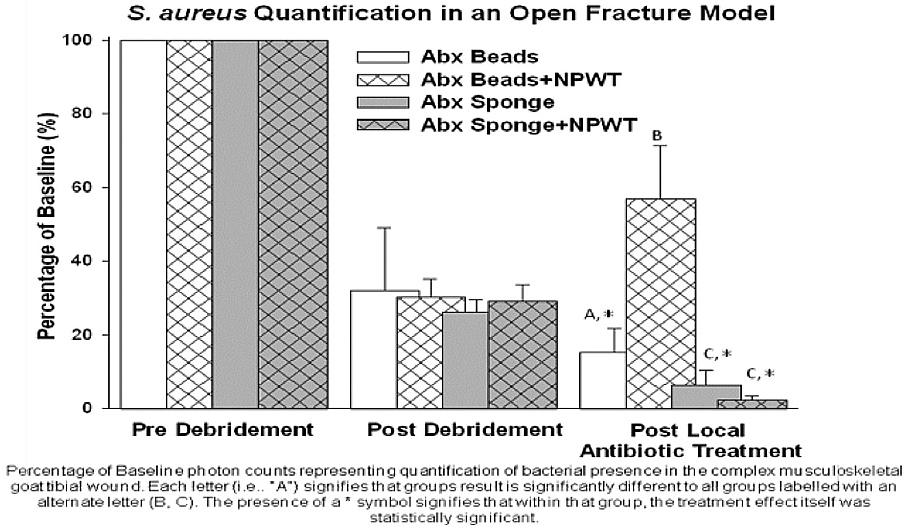
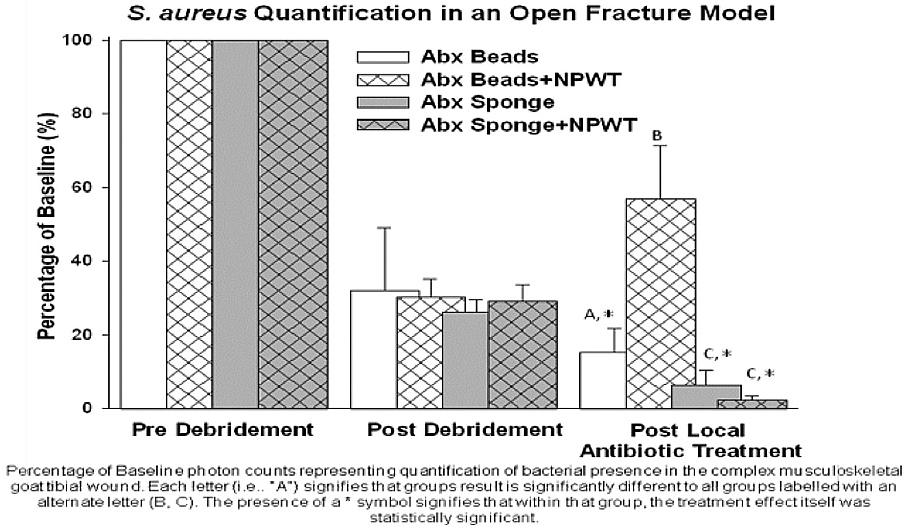
Methods: The effectiveness of PMMA antibiotic beads was compared to antibiotic loaded chitosan sponge, used in both wound pouch and NPWT modalities. A complex tibial open fracture wound was created in goats and inoculated with Staphylococcus aureus. The wounds were débrided at 6 hours, and the bacteria was quantified both pre- and postdébridement. The animals were assigned to a group, and the bacteria within the wound were requantified after 2 days. The four groups were: antibiotic bead pouch, antibiotic beads with NPWT, chitosan sponge pouch, and chitosan sponge with NPWT. Both the beads and sponges contained vancomycin.
Results: There were significantly fewer bacteria within the wounds treated with chitosan sponge compared with antibiotic beads irrespective of use in a pouch or with NPWT. Unlike beads, the effectiveness of chitosan sponges was not reduced by NPWT.
Conclusion: This study demonstrates that a biodegradable chitosan sponge loaded with vancomycin is superior to antibiotic-impregnated beads at eradicating S. aureus in a complex large animal wound model, whether used in conjunction with NPWT or in a wound pouch. It also offers advantages in handling, antibiotic choice, device removal, and its effect is not reduced when used with NPWT. We believe that the sponge is more effective because more surface area is in contact with the wound surface where the antimicrobial agents can act. PMMA beads act as a depot, eluting antibiotic that must diffuse throughout the wound. When used with NPWT, the antibiotic is removed before it can reach the bacteria not in contact with the beads. The increased contact with the wound surface of the chitosan sponge allows improved antimicrobial action both with and without NPWT, and the difference in effectiveness is more pronounced with NPWT. Animal Statement: This study has been conducted in compliance with the Animal Welfare act, the implementing Animal Welfare Regulations, and the principles of the Guide for the Care and Use of Laboratory Animals.
Disclaimer: The opinions and assertions contained herein are the private views of the authors and are not to be construed as official or as reflecting the views of the Department of the Army or Department of Defense.
Alphabetical Disclosure Listing (808K PDF)
• The FDA has not cleared this drug and/or medical device for the use described in this presentation (i.e., the drug or medical device is being discussed for an “off label” use). ◆FDA information not available at time of printing. Δ OTA Grant.