Fri., 10/5/12 Foot & Ankle, PAPER #48, 11:04 am OTA-2012
A Comparison of Weight-Bearing Protocols and Outcomes for Syndesmotic Ankle Fixation: 6 Weeks Versus 12 Weeks
Jeffrey E. McAlister, DPM; Jeff E. Schulman, MD; Noah Oliver, DPM;
A. Stephen Malekzadeh, MD; Cary A. Schwartzbach, MD; Matthew S. Levine, MD; Daniel Dziadosz, MD; Robert Hymes, MD;
Orthopedic Trauma Program, INOVA Fairfax Hospital, Falls Church, Virginia, USA
Purpose: This retrospective analysis was designed to evaluate two weight-bearing protocols, 6 weeks versus 12 weeks of non–weight bearing (NWB), following syndesmotic fixation at a Level I trauma center. The primary outcome measure was failure of syndesmotic reduction. Our hypothesis was that there would be no significant difference between the two postoperative protocols.
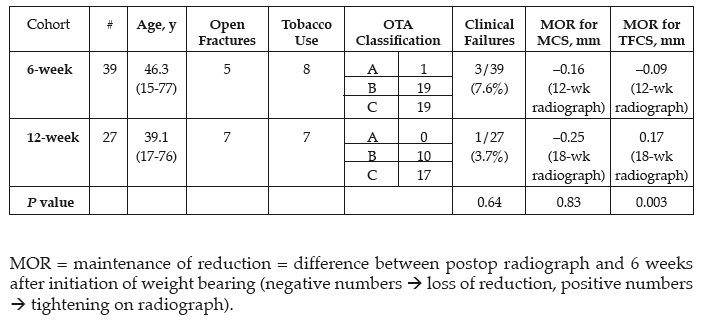
Methods: All patients with syndesmotic injuries (with and without associated ankle fracture) who underwent operative fixation at a Level I trauma center between February 2007 and September 2010 were reviewed. Data, including age, mechanism of injury, and other demographics, were extracted from the medical record. Radiographs were evaluated preoperatively, immediately postoperatively, and at 2, 6, 12, and 18 weeks postoperatively for tibiofibular clear space (TFCS) and medial clear space (MCS). Key study measurements were defined as those measured from immediate postoperative radiographs and those taken 6 weeks after the initiation of weight bearing (12 weeks vs 18 weeks postoperatively for the 6- and 12-week cohorts, respectively). Clinical failure was defined as complete loss of reduction requiring revision surgery. Data were statistically compared using a two-tailed paired t test and Fisher exact test with significance set to P <0.05.
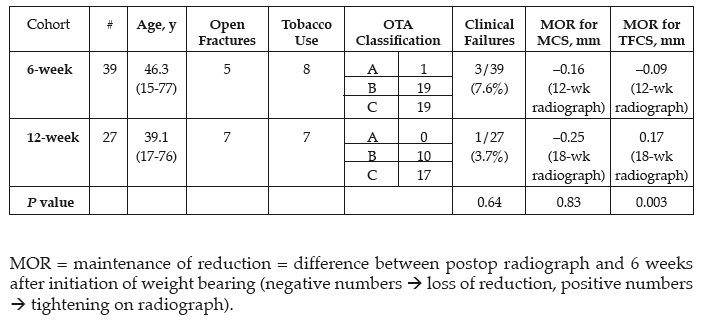
Results: 146 syndesmoses were repaired during the data collection period. 100 had complete clinical follow-up and of these, 66 had complete data for radiographic evaluation. Three patients from the 6-week cohort and one from the 12-week cohort failed clinically and went on to early surgical revision. Radiographic comparison revealed no statistical difference between the maintenance of reduction (MOR) for the MCS (–0.16 mm vs –0.25 mm, P = 0.83) whereas there was statistical significance for the MOR of the TFCS (–0.09 mm vs 0.17 mm, P = 0.003).
Conclusion: This retrospective review is the first of its kind to compare two postoperative weight-bearing protocols after syndesmotic fixation. We demonstrated statistical significance for maintenance of TFCS with a longer postoperative non–weight-bearing period, but no significance for MCS. Some literature suggests that MCS may be more clinically relevant. Despite this, we question whether there is true clinical significance in either of these cohorts given the magnitude of difference being measured on radiographs (<0.5 mm). Ultimately, the number of true clinical failures was low in both cohorts with no statistical significance (7.6% vs 3.7%, P = 0.64). We feel that weight bearing at 6 weeks after surgical repair of a syndesmosis is a viable option, particularly in certain patient populations that may benefit most from an earlier return to activity.
Alphabetical Disclosure Listing (808K PDF)
• The FDA has not cleared this drug and/or medical device for the use described in this presentation (i.e., the drug or medical device is being discussed for an “off label” use). ◆FDA information not available at time of printing. Δ OTA Grant.