Fri., 10/5/12 Foot & Ankle, PAPER #45, 10:46 am OTA-2012
Δ Can We Tell If the Syndesmosis is Reduced Using Fluoroscopy?
Paul Tornetta III, MD; Scott Koenig, MD; Gabriel Merlin; Yelena Bogdan, MD;
Boston University Medical Center, Boston, Massachusetts, USA
Background/Purpose: Reduction of the ankle mortise correlates with outcomes for unstable ankle fractures. Increased emphasis has been placed on the reduction of the syndesmosis as well as not missing subtle syndesmotic injury. Several authors have highlighted the use of lateral views to aid in determining if the fibula is in its proper position with respect to the tibia. The purpose of this study was to evaluate the ability of surgeons to determine if the fibula is reduced, anteriorly displaced, or posteriorly displaced based on fluoroscopic images by comparison with the known normal for both the ipsilateral and contralateral ankles.
Methods: Perfect lateral radiographs of both ankles were obtained in 7 cadaveric specimens (14 ankles). These were confirmed by two evaluators independently rotating an image intensifier until the plafond had only one clear surface. In all cases, the angulation was <2° different, confirming the ability to predictably obtain a “perfect lateral.” After saving these images, a Kirschner wire (K-wire) was placed in both the distal tibia and the distal fibula to be used later to measure fibular translation. The deltoid and syndesmotic ligaments were then sectioned and the fibula was translated 2.5 mm and 5 mm in the anterior and posterior directions by changing the distance between the K-wires with calipers for a precise displacement. A perfect lateral radiograph was taken at each displacement and saved (5 images/side). Each ankle was used as a case consisting of a “normal” image, followed by 10 randomly selected images (random number generator). These images could be taken from the ipsilateral or contralateral ankle for that specimen and could be any of the 10 images. Images could also be repeated (random generator). Within each set of 10 images, the initial “normal” image and the contralateral ankle “normal” image were always included to test for ability to determine the reduced position. Four orthopaedic trauma fellowship–trained surgeons from different Level I centers reviewed each case. They were asked to compare the 10 images to the normal image and determine if the fibula was “reduced,” “displaced anteriorly,” or “displaced posteriorly.” The ability of the surgeons to identify displacement and interobserver reliability were assessed for the 560 test images.
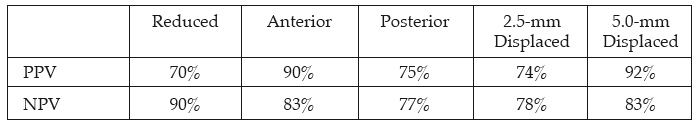
Results: See table below for summary. The surgeons were better able to identify malreduction than reduction, with negative predictive values (correctly identifying malreduction) of 95% for ipsilateral ankle images and 85% for contralateral images. The overall sensitivity for reduction was 94% for the ipsilateral ankle but only 68% for the contralateral ankle, although the range was great among reviewers (32%-100%). Anterior displacement was easier to see than posterior displacement (positive predictive value [PPV] = 90% vs 77% for ipsilateral and 90% and 71% for contralateral). Greater displacements were easier to see with PPV for 2.5 mm and 5.0 mm being 76% and 93% for ipsilateral and 71% and 91% for contralateral ankles. All reviewers had the most difficulty with 2.5 mm of posterior displacement, correctly identifying posterior malreduction in 27% to 64%. The overall agreement between reviewers (using Kappa values) was excellent for anterior displacement (0.71) and for displacements of 5 mm in either direction (0.75), and only moderate for the other displacements and for the reduced position (0.51-0.6). The overall PPV and negative predictive value (NPV) for various displacements is shown in the table.
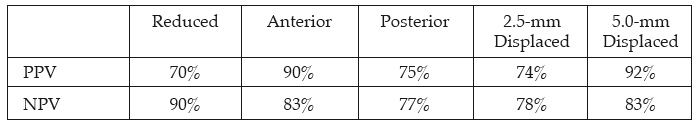
Conclusion: Four experienced trauma surgeons evaluated known translational displacements of the fibula against the normal ankle radiographs using a verified perfect lateral view. Their ability to determine malreduction was 90%, but their ability to confirm reduction was only 70%. Minor posterior displacement was the most difficult to identify. While it is unknown how much translational displacement of the syndesmosis is acceptable, it seems that experienced surgeons will most often be able to reduce the joint within 2.5 mm and that fluoroscopic comparisons to the normal ankle are helpful in determining malreduction.
Alphabetical Disclosure Listing (808K PDF)
• The FDA has not cleared this drug and/or medical device for the use described in this presentation (i.e., the drug or medical device is being discussed for an “off label” use). ◆FDA information not available at time of printing. Δ OTA Grant.