Fri., 10/5/12 Foot & Ankle, PAPER #41, 10:12 am OTA-2012
Does the Fibula Need to Be Fixed in Complex Pilon Fractures?
John C. Kurylo, MD; Neil Datta, Kendra N. Iskander, MD, MPH; Paul Tornetta, III, MD;
Boston University Medical Center, Boston, Massachusetts, USA
Background/Purpose: The classic teaching is that fixation of the fibula should be the first step in the surgical tactic for complex pilon fractures. However, with the advent of staged protocols including external fixators to maintain length and low-profile locked fixation it may not be necessary. The purpose of this study is to evaluate the effect of fibula fixation on alignment and complications in high-energy pilon fractures with tibial metadiaphyseal dissociation.
Methods: From 364 patients with plafond fractures, 111 had high-energy injuries with metadiaphyseal dissociation and form the basis of the study. We identified three groups that had open reduction and internal fixation (ORIF) of the distal tibia: those with a fibula fracture that was fixed (26), those with a fibula fracture that was not fixed (37), and those without a fibula fracture (30). A fourth group of patients in whom the tibial metaphyseal reduction was supported definitively by external fixation (typically because the skin was not deemed amenable to surgical intervention) was reviewed to evaluate the effect of ORIF of the distal tibia in supporting the metaphysis. The radiographs and charts were reviewed for fracture characteristics; metaphyseal alignment at presentation, after fixation, and at union; surgical procedures; and complications. Complications included infection, fusion, hardware removal, compartment syndrome, and nonunion. A statistician performed comparisons among the groups. We compared complication rates and the alignment of patients with fibula fractures fixed to those who were not fixed and used patients without a fibula fracture as a control group to benchmark the results. The reason for fibula fixation, when chosen, was documented.
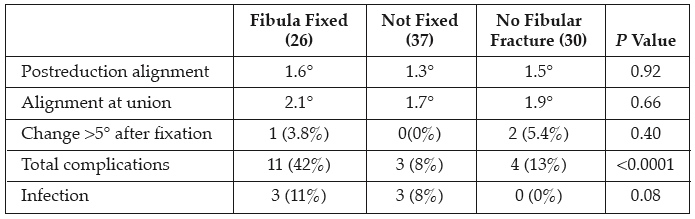
Results: Patients’ average age was 42 years (range, 18-85) with 77 men and 34 women. There were no differences in patient demographics, fibula fracture pattern (oblique, transverse, or comminuted), or location (A, B, or C). There were 25 (23%) open fractures, all with a fibula fracture (P = 0.004). Initial external fixation was used in 95 patients (85%). 60% of the plafond fixation was locked and no difference was found between the groups (P = 0.4). Patients with initial valgus deformity were more likely to have their fibula fixed than those presenting in varus (P = 0.0015). Of the 26 who had fibular fixation, 11 were staged at an average of 17 days after initial external fixation for inability to hold length or alignment in the frame. The other 15 were fixed at the time of the definitive plafond fixation to augment fixation (6), for soft-tissue prominence of the displaced fibula (3), or to aid in the reduction (6). We compared the overall alignment, maintenance of alignment, and complications among these groups (table). There was no difference in the ability to obtain a reduction or to maintain it to union when the fibula was or was not fixed (P = 0.5). Neither group with fibula fractures had different alignment than the group without a fibula fracture (P = 0.92). There was a higher overall complication rate if the fibula was fixed (P <.0001). In the definitive external fixation group, 9 of 18 were open and 11 had fibular fixation to maintain length during their course. There were 15 complications in these 18 patients including 8 nonunions, 3 infections, 3 fusions, and 1 hardware removal. The average malalignment in this group at union or reintervention was 7° and different than those that had ORIF of the distal tibia (P <.001). In contradistinction, union was achieved in all cases treated with ORIF of the tibia. The use of locking plates (P = 0.8) did not affect the overall change in alignment during healing.
Table. Alignment as average absolute values, and complications in the groups that had tibial fixation
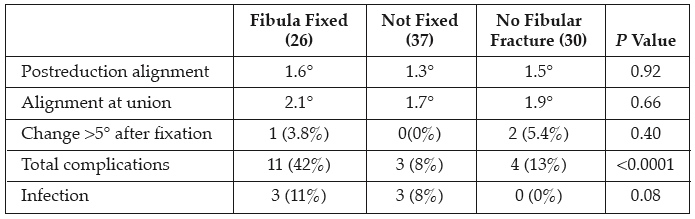
Conclusion: Although it may be helpful in specific cases to augment initial external fixation or to aid in reduction, fibular fixation is not a necessary step in the reconstruction of pilon fractures. We found a higher rate of complications if the fibula was fixed (P 0<.0001), without any benefit to reduction or maintenance of alignment. Finally, the use of external fixation as definitive support for the metaphyseal alignment resulted in a high percentage of nonunions (44%) and a more angular deformity than if plated.
Alphabetical Disclosure Listing (808K PDF)
• The FDA has not cleared this drug and/or medical device for the use described in this presentation (i.e., the drug or medical device is being discussed for an “off label” use). ◆FDA information not available at time of printing. Δ OTA Grant.