Fri., 10/14/11 Tibia, Paper #54, 11:49 am OTA-2011
Δ The Role of Antibiotics in Open Fractures Revisited: Characteristics of Staphylococcus aureus (SA) and Susceptibility Profile
Carla C. Saveli, MD; Steven J. Morgan, MD; Robert W. Belknap, MD; Erin Ross, BS;
Philip F. Stahel, MD; David J. Hak, MD; Walter L. Biffl, MD; George W. Chaus, MD;
Connie S. Price, MD;
Denver Health Medical Center, University of Colorado School of Medicine,
Denver, Colorado, USA
Purpose: The benefits of antibiotic prophylaxis in open fractures have been clearly demonstrated in several randomized controlled trials, but the choice of antibiotic remains controversial since the current guidelines do not recommend agents with methicillin resistant SA (MRSA) activity. Our objective was to develop preliminary data on the incidence of SA colonization and surgical-site infections (SSIs) in orthopaedic trauma patients with open fractures who receive standard antibiotic prophylaxis compared to a regimen including targeted MRSA coverage.
Methods: In order to compare the safety and benefits of adding MRSA coverage to standard antibiotic prophylaxis, a randomized prospective clinical trial was performed. Between April 2009 and June 2011, all consecutive adult patients who presented to the emergency department (ED) with an open fracture and met study criteria were included. Patients were randomly allocated to receive either cefazolin alone (control arm) or vancomycin and cefazolin (experimental arm) from presentation to the ED until 24 hours after the surgical intervention. Screening for SA carriage was performed with nares swabs, predébridement, and postdébridement open fracture wound swabs. Standard surgical management of the open fractures involved surgical débridement and fracture stabilization. Patients underwent prospective assessment for the development of SSI within 30 days of the initial surgery.
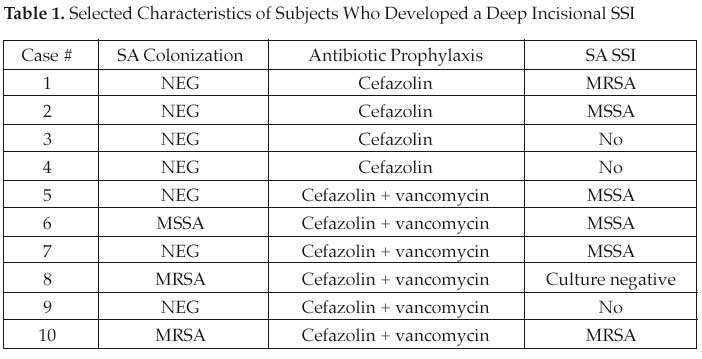
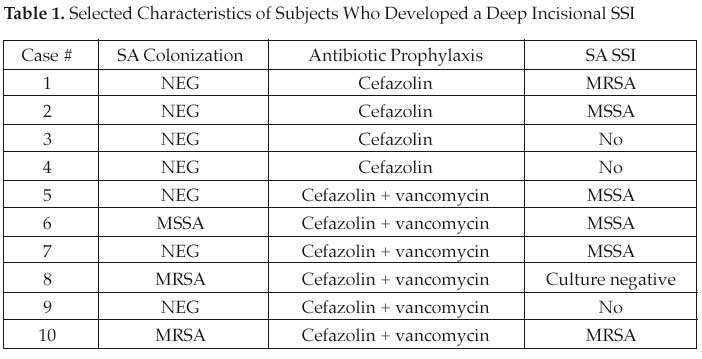
Results: 132 patients with an open fracture were randomized to one of the prophylactic antibiotic regimens. Study demographics and baseline characteristics were balanced between the two groups. 24% of the subjects were identified as colonized with SA. The prevalence of methicillin-sensitive SA (MSSA) and MRSA colonization among the sample were 21% and 4%, respectively. The overall rate of SSI was 16% (16/106)—6 superficial and 10 deep incisional. Selected characteristics of patients who developed a deep incisional SSI are summarized in Table 1. No adverse or severe adverse events in either of the study arms were reported during the study period.
Conclusions: Preliminary findings demonstrate that addition of vancomycin to standard antibiotic prophylaxis is safe. SA colonization in orthopaedic trauma patients is similar to the general population and methicillin resistance was shown in 4% of these patients. SA was a causative pathogen in 60% of the deep incisional SSIs and MRSA accounted for 20% of them. Further data are needed to determine whether the addition of vancomycin to standard antibiotic prophylaxis prevents the development of SSI compared to standard regimens.
Alphabetical Disclosure Listing (628K PDF)
• The FDA has not cleared this drug and/or medical device for the use described in this presentation (i.e., the drug or medical device is being discussed for an “off label” use). ◆FDA information not available at time of printing. Δ OTA Grant.