Fri., 10/14/11 Pelvis & Spine, Paper #45, 10:40 am OTA-2011
Critical Analysis of Pelvic Angiography for Trauma and Development of a Scoring System
Maria Iannolo, MD; Jonathan M. Gross, MD; Catherine A. Humphrey, MD;
Mark L. Prasarn, MD; John P. Ketz, MD; John T. Gorczyca, MD
University of Rochester Medical Center, Rochester, New York, USA
Purpose: The purpose of this study is to critically assess the indications used for pelvic angiography and embolization at a trauma center over a 7-year period, and to identify pre-procedure factors associated with arterial hemorrhage.
Methods: Review of medical records revealed 44 patients with pelvis fractures had pelvic angiography over 7 years. The average age was 53.1 years and the mean ISS was 25.5. Medical records were reviewed for patient age, hemodynamic status, transfusions received, contrast extravasation (“blush”) on CT scan, laboratory values, and associated injuries. The fractures were classified according to the Young-Burgess and OTA classification systems.
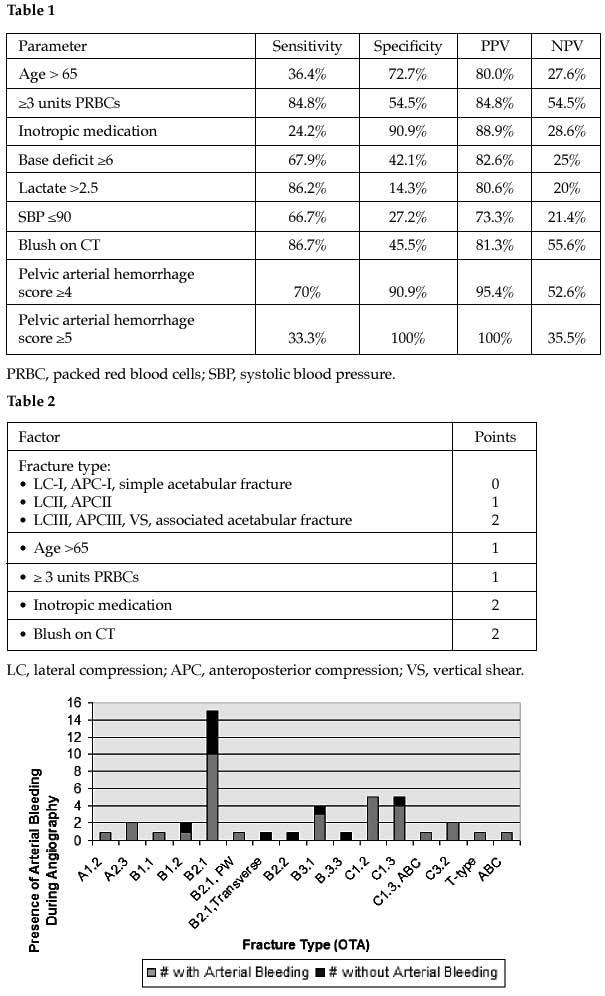
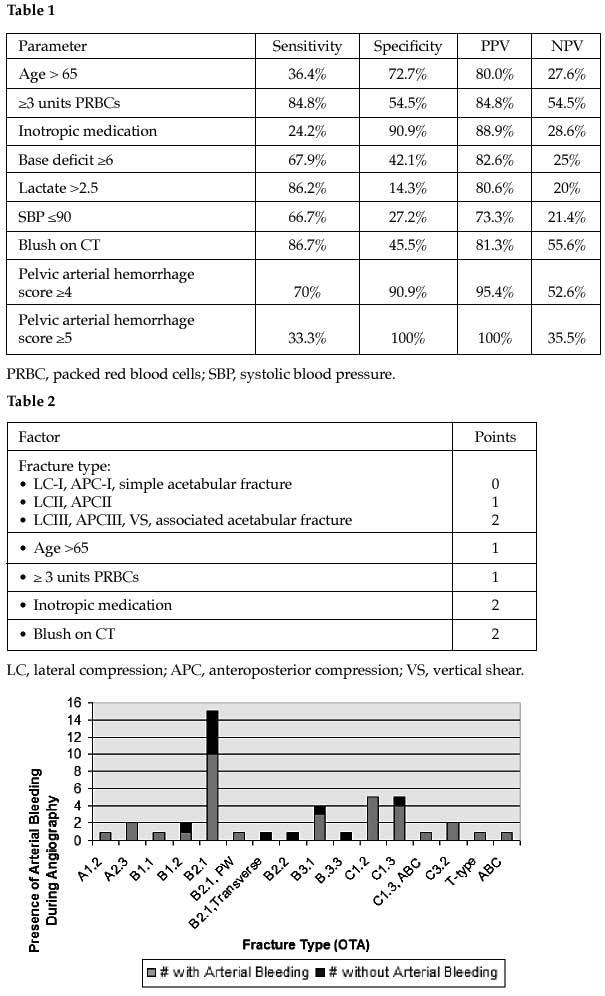
Results: 33 of 44 patients (75%) had active arterial hemorrhage and all had embolization performed. 11 patients did not have arterial hemorrhage, yet the interventional radiologist performed embolization in 7 (64%). In 7 additional patients, selective embolization of the bleeding vessel was not done, and instead the entire internal iliac artery was embolized. Patients who were transfused ≥3 units of blood and patients with contrast extravasation on CT scan had significantly greater risk of arterial hemorrhage at angiography (P = 0.016, P = 0.042). The presence of hypotension (systolic blood pressure ≤90), abnormal laboratory values (base deficit, lactate), and receipt of inotropic medication were found to have a nonsignificant correlation with the presence of arterial bleeding (see Table 1). Arterial hemorrhage was present in 66% (19 of 29 patients) with OTA type A/B fractures, and in 92% (12 of 13) with OTA type C fractures (see figure) (P = 0.13). Branches of the internal iliac artery were injured in 28 of 33 cases (85%) compared with branches of the external iliac artery in 8 cases (24%). Patients >65 years were more likely to have arterial hemorrhage despite sustaining a less severe fracture. Based on the above findings, we have developed a scoring system based on 5 categories: fracture type, age >65 years, receipt of inotropic medication, number of packed red blood cell units transfused, and contrast extravasation on CT scan (Table 2). A score ≥4 had a positive predictive value of 95% for the presence of arterial hemorrhage.
Conclusions: Selective embolization should be used when possible to avoid devascularization of important structures. The scoring system presented predicts the presence of arterial hemorrhage at angiography.
Alphabetical Disclosure Listing (628K PDF)
• The FDA has not cleared this drug and/or medical device for the use described in this presentation (i.e., the drug or medical device is being discussed for an “off label” use). ◆FDA information not available at time of printing. Δ OTA Grant.