Fri., 10/14/11 Pelvis & Spine, Paper #44, 10:29 am OTA-2011
Can a Single Screw Be Used for Bilateral Sacroiliac Fixation?
Jason A. Patterson, MD1; Alex McLaren, MD1; Patrick Liu, MD2; Ryan McLemore, MD1;
1Banner Good Samaritan Medical Center, Phoenix, Arizona, USA;
2Mayo Clinic Phoenix, Phoenix, Arizona, USA
Purpose: Screw fixation of the sacroiliac (SI) joint is a well established technique. The ideal screw path across one SI joint is not coincident with the ideal path across the contralateral joint. It is hypothesized that there is sufficient space for a straight line path across both SI joints to place a bilateral screw in both the S1 and S2 segments.
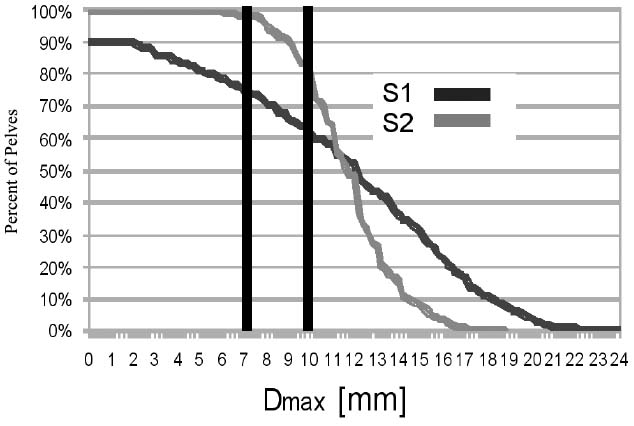
Methods: 432 pelvic CT scans were processed to obtain high-definition 3-dimensional (3D) digital models of the pelvis at the S1 and S2 segments. Bone cortex was identified by voxel density producing a 3D mesh of the cortical contours. S1 and S2 were analyzed similarly. A straight line path was digitally placed within the cortical contours of the sacral segment, and extended from the outer table of one posterior ilium, across the SI joint through the S1 or S2 sacral segment, across the opposite SI joint, and out the opposite posterior ilium. The diameter of the path was increased until it contacted cortex geometrically defining the position, alignment, and maximum diameter (Dmax) of the single path across either the S1 or S2 segment. The Dmax available for a screw was documented for S1 and S2 and was associated with gender, age, and body mass index (BMI). 10 mm was defined as the smallest diameter in which a skilled surgeon could consistently and safely place a 7.3-mm screw, allowing a 2.7-mm margin for error. Binomial logistic regression was used to associate the path diameter with gender, age, and BMI with α <0.05.
Results: 49% of pelves had 10 mm or more at both the S1 and S2 segments. 67% had 10 mm or more in S1 only and 76% had 10 mm or more in S2 only. In 6% of pelves, neither S1 nor S2 had a 10-mm path for the bilateral screw. 15% of S1s had <7 mm. Dmax was smaller in females than in males at S1 (P = 0.049) and S2 (P <0.001) but did not associate with age or BMI.
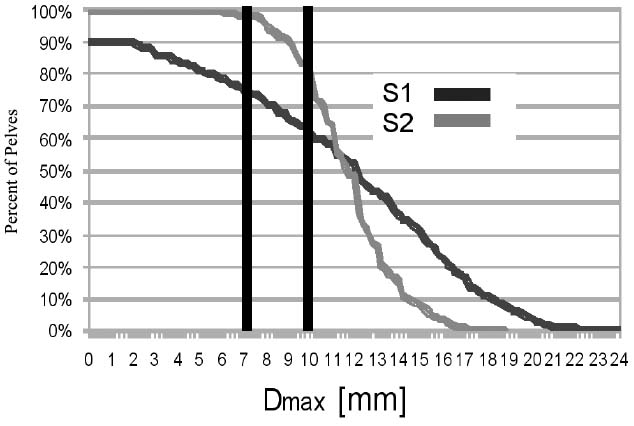
Conclusions: One in three pelves (33%) lacked sufficient bone to pass a bilateral screw across both SI joints in the S1 segment, one in four (24%) lacked sufficient bone to pass a bilateral screw across the S2 segment, and 6% lacked sufficient bone in both the S1 and S2 segments. Separate unilateral SI screws on each side may be safer than a long bilateral screw traversing both SI joints when experience with this procedure is limited.
Alphabetical Disclosure Listing (628K PDF)
• The FDA has not cleared this drug and/or medical device for the use described in this presentation (i.e., the drug or medical device is being discussed for an “off label” use). ◆FDA information not available at time of printing. Δ OTA Grant.