Thurs., 10/13/11 Basic Science, Paper #35, 4:30 pm OTA-2011
•Local Antibiotic Delivery by a Bioabsorbable Gel is Superior to PMMA Beads at Reducing Infection in an Open Fracture Model
Jowan G. Penn-Barwell, MRCS1,2; Clinton K. Murray, MD3; Joseph C. Wenke, PhD1;
1US Army Institute of Surgical Research, Fort Sam Houston, Texas, USA;
2Academic Dept. of Military Surgery and Trauma, Royal Centre for Defense Medicine,
Birmingham, United Kingdom;
3Brooke Army Medical Center, Fort Sam Houston, Texas, USA
Purpose: Infection remains a common complication of open fracture despite the use of systemic antibiotics. Local delivery potentially allows a high concentration of antibiotics to be achieved in the wound, thus avoiding the side effects and cost associated with systemic administration. Beads molded from polymethylmethacrylate (PMMA) arthroplasty cement are currently the clinical standard for local antibiotic delivery. However, PMMA beads are not the ideal local antibiotic vehicle; they are bulky and not bioabsorbable, therefore complicating closure and requiring surgical removal. Moreover, they are merely a depot and do not cover the entire surface of the wound. The purpose of this study was to evaluate whether a phospholipid gel might be a superior local antibiotic vehicle to PMMA beads.
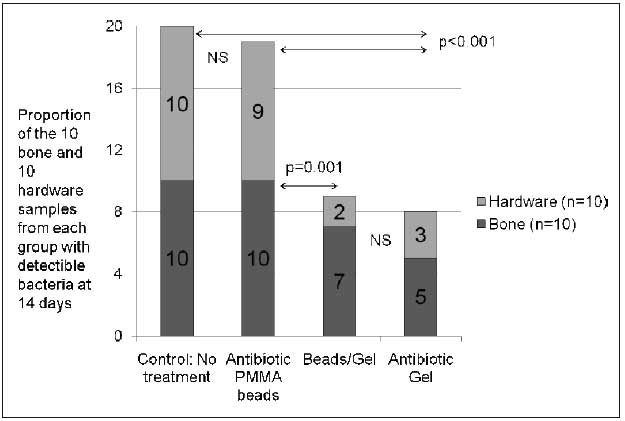
Methods: This study used a segmental defect rat model contaminated with Staphylococcus aureus and treated with similar amounts of local antibiotics delivered by gel or PMMA beads. The gel, called DFA-02, was a phospholipid vehicle containing 1.7% vancomycin and 1.9% gentamicin by weight. These antibiotics are eluted to a peak tissue concentration between 1 and 8 hours and sustained above the S. aureus mean inhibitory concentration for 5 days. PMMA beads were manufactured using a standard technique with commercial PMMA cement and 3.3% vancomycin and 4% tobramycin by weight. Tobramycin was used instead of gentamicin as this is the aminoglycoside used in PMMA beads in the US. In the gel group, 1 mL of DFA-02 was spread throughout the wound, a total of approximately 36 mg of antibiotics. In the bead group, four 3-mm beads were placed in the wound, 2 in the defect and 2 in the adjacent tissue envelope—a total of 60 mg of antibiotics. A combined beads/gel group received half of both treatments in each wound and a control group received no antibiotics. After 14 days, bone and hardware was harvested for separate microbiologic analysis. The outcome measure was the presence and quantification of bacteria on bone or hardware at this point.
Results: These results show that there was a significantly lower infection rate in groups treated with antibiotics delivered by gel compared with those treated with either antibiotic beads or no antibiotics at all. Quantitative cultures also demonstrate significantly less bacteria in the wounds that were treated with the gel (P = 0.001).
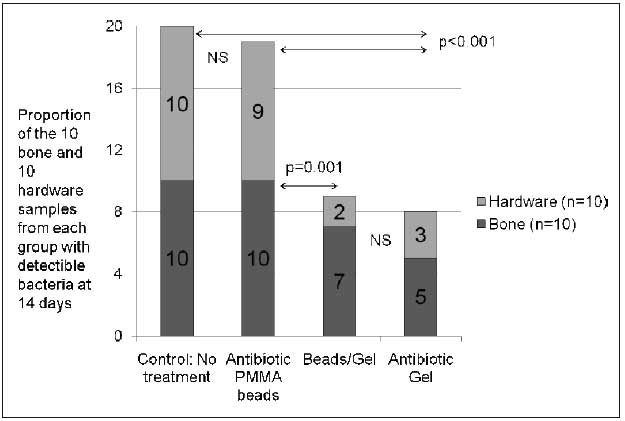
Conclusion: These results indicate that local antibiotics are superior at reducing infection when delivered in a gel rather than by beads. It is believed that the ability to apply the gel to all areas of the wound caused high levels of antibiotics throughout the wound. The beads are a local depot that has a concentration gradient within the wound. In animals treated with antibiotic beads, only some areas of the wound may be exposed to enough antibiotics to kill the bacteria, particularly those that are within a biofilm. This study demonstrates that local antibiotic delivery vehicles that cover the entire wound bed may be more effective at reducing infection.
Disclaimer: The opinions and assertions contained herein are the private views of the authors and are not to be construed as official or as reflecting the views of the Department of the Army or Department of Defense.
Alphabetical Disclosure Listing (628K PDF)
• The FDA has not cleared this drug and/or medical device for the use described in this presentation (i.e., the drug or medical device is being discussed for an “off label” use). ◆FDA information not available at time of printing. Δ OTA Grant.