Thurs., 10/13/11 Basic Science, Paper #32, 4:12 pm OTA-2011
Early Initial Antibiotics and Debridement Independently Reduce Infection in an Open Fracture Model
Jowan G. Penn-Barwell, MRCS1,2; Clinton K. Murray, MD3; Joseph C. Wenke, PhD1;
1US Army Institute of Surgical Research, Fort Sam Houston, Texas, USA;
2Academic Dept. of Military Surgery and Trauma, Royal Centre for Defense Medicine,
Birmingham, United Kingdom;
3Brooke Army Medical Center, Fort Sam Houston, Texas, USA
Purpose: Open fractures are common, and infection frequently complicates these injuries. Despite this, there is still controversy and uncertainty regarding the urgency of initial treatment. The majority of animal studies indicate that early irrigation and débridement reduces infection; unfortunately, these studies often do not involve antibiotics. Clinical studies indicate that early antibiotic administration may be beneficial but suggests that the timing of initial débridement does not affect the infection rate. These studies are all observational or retrospective and are fraught with confounding variables. The purpose of this study was to control for these variables using an animal model incorporating both systemic antibiotics and surgical treatment.
Methods: This study used a segmental defect rat model contaminated with Staphylococcus aureus and treated with a - day course of systemic cefazolin (5 mg/kg 12 hourly) and surgical treatments, both of which were initiated independently at 2, 6, and 24-hour time points. After 14 days, bone and hardware was harvested for separate microbiologic analysis. The outcome measure was whether bacteria was detectible on bone or hardware at this point.
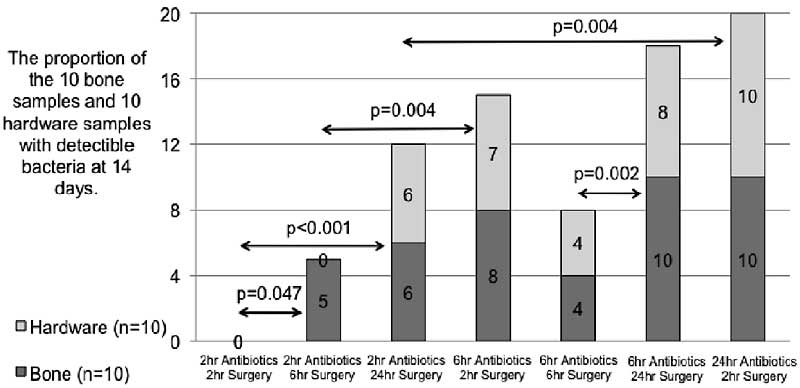
Results: These results show that the earlier systemic antibiotic treatment or surgery is initiated, the more infection is reduced, and their effect is independent of each other and are synergistic. When antibiotics are started at 2 hours, delaying surgical treatment from 2 to 6 hours significantly increases infection (P = 0.047). However, delaying surgery to 24 hours increases infection, but not significantly (P = 0.054). In order to determine which had a more temporally significant effect on bacteria, antibiotics or surgery, two pairs of “mirrored” study groups were compared, first a pair of groups in which the timing of surgery and antibiotics was reversed around the 2 and 6-hour time points, and second in which treatments occurred at 2 and 24 hours. In both comparisons, the timing of antibiotics had a more significant effect on the proportion of positive samples than earlier surgery. At the 2 and 6-hour treatments, the P value was 0.004 and for the 6 and 24 timings, it was 0.003.
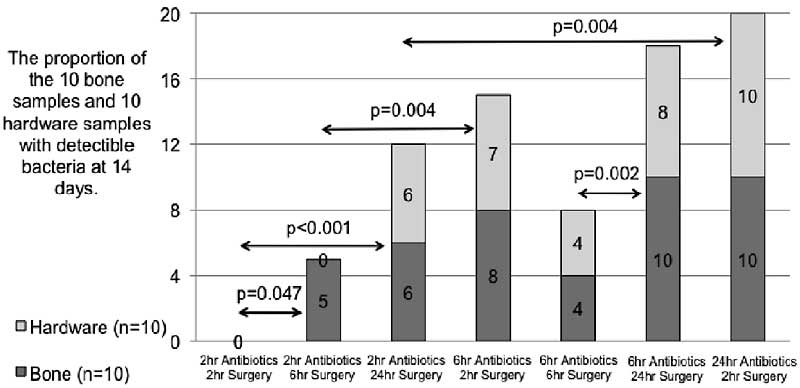
Conclusion: Surgery and antibiotics at 2 hours completely eradicates the bacteria, but surgical delay for 6 hours appears to allow the bacteria to form nonsusceptible colonies. Further delaying surgery until 24 hours does not appear to affect the infection rate. Delaying antibiotics to 6 or 24 hours had a profound detrimental effect on the infection rate regardless of timing of surgery. These findings are consistent with the concept that bacteria progress from a vulnerable planktonic form to a treatment-resistant biofilm.
Disclaimer: The opinions and assertions contained herein are the private views of the authors and are not to be construed as official or as reflecting the views of the Department of the Army or Department of Defense.
Alphabetical Disclosure Listing (628K PDF)
• The FDA has not cleared this drug and/or medical device for the use described in this presentation (i.e., the drug or medical device is being discussed for an “off label” use). ◆FDA information not available at time of printing. Δ OTA Grant.