Thurs., 10/8/09 Pelvis & Acetabulum, Paper #38, 4:50 pm OTA-2009
Impact of a 3-Dimensional “Hands-On” Anatomical Teaching Module on Acetabular Fracture Pattern Recognition by Orthopaedic Residents: A Pilot Study
Erik Hansen, MD (n); Meir Marmor, MD (n); Amir Matityahu, MD (n);
University of California San Francisco, San Francisco General Hospital,
San Francisco, California, USA
Purpose: This prospective pilot project was designed to determine the efficacy of a “hands on” three-dimensional anatomical model to teach orthopaedic surgical residents the correct identification of acetabular fracture patterns, fixation techniques, and surgical approaches. Our hypothesis was that active learning using these models would improve the short-term diagnostic accuracy of orthopaedic residents when compared to standard teaching methods.
Methods: Ten standard Sawbones pelvi were used, each depicting one of the classic fracture patterns described by Judet and Letournel. The right acetabulum was “osteotomized” and fixed in a distracted manner by threaded Kirschner wires to recreate the distinct fracture pattern. On the left acetabulum, the fracture was drawn and “fixed” in a standard manner using pelvic plates and screws. 25 orthopaedic surgery residents were recruited for the study. The residents were divided into 2 equal groups based on year-in-training (YIT). Residents in group 1 were asked to study acetabular fracture classification using specially made information sheets that included all relevant materials tested. Group 2 was asked to study using the same sheets with the addition of the acetabular models. Pre- and postintervention quizzes, based on representative radiographs and axial CT images, were administered to determine the impact of each intervention on acetabular fracture and fixation pattern recognition.
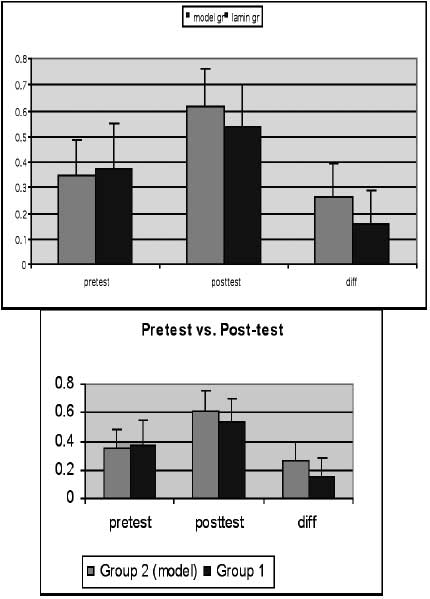
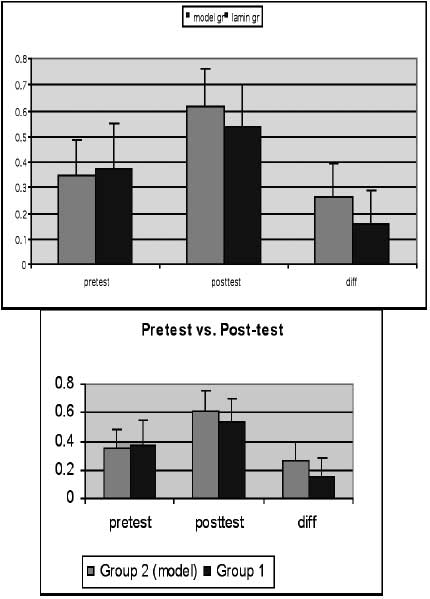
Results: The mean preintervention quiz scores were as follows: 1st year residents, 27 ± 8%; 2nd year residents, 27 ± 14%; 3rd year residents, 36 ± 12%; 4th year residents, 52 ± 3%; and 5th year residents, 48 ± 3%. The correlation between preintervention quiz and YIT was R = 0.94. The mean postintervention scores were higher for all residents: 1st year residents, 50 ± 21%; 2nd year residents, 54 ± 2%; 3rd year residents, 61 ± 10%; 4th year residents, 71 ± 12%; and 5th year residents, 58 ± 16%. Group 1 scores significantly increased from a mean of 37.6 ± 17.6% to 53.5 ± 16.7% (P = 0.0001), while group 2 scores significantly increased from a mean of 35.0 ± 13.6% to 61.4 ± 14.5%(P = 4.75 • 10-5). Both groups improved following the intervention. However, the relative improvement of group 2 was significantly higher than group 1 (26.4% vs 15.9%, P = 0.04).
Conclusion: The use of a three-dimensional teaching module improves the diagnostic accuracy of orthopaedic residents to correctly identify acetabular fracture patterns and methods of fixation. This intervention seems to have the largest impact on residents who are in their first 3 years of training.
• The FDA has not cleared this drug and/or medical device for the use described in this presentation (i.e., the drug or medical device is being discussed for an “off label” use). ◆FDA information not available at time of printing. Δ OTA Grant