OTA 2013 Posters
Scientific Poster #32 Geriatric OTA 2013
Geriatric Hip Fractures and Intra-Hospital Testing: Predicting Costs Utilizing the ASA Score
Vasanth Sathiyakumar, BA; Jordan C. Apfeld, BA; Young M. Lee, BS; Daniel Sutton, BS;
Jesse M. Ehrenfeld, MD, MPH; Benjamin Hooe, BS; William T. Obremskey, MD, MPH; Manish K. Sethi, MD;
Vanderbilt University, Nashville, Tennessee, USA
Background/Purpose: Surgical fixation of low-energy hip fractures in the elderly is a common orthopaedic procedure that is expected to increase in frequency. As America moves toward alternative systems of payment in which providers and hospitals will be paid a singular amount for care of a patient or injury, it is pivotal that orthopaedic trauma surgeons better understand patient factors that influence intra-hospital testing. Prior data have demonstrated the utility of the American Society of Anesthesiologists (ASA) physical status classification score in predicting postoperative length of stay (LOS) in geriatric hip fractures. This study goes further in exploring the potential use of the ASA score in predicting hospital resources utilized by geriatric hip fracture patients during their perioperative hospital admission.
Methods: From January 1, 2000 to December 31, 2009, all patients over the age of 60 years who presented to the only Level I trauma center in a large metropolitan area with an isolated low-energy hip fracture were reviewed. A total of 720 patients were identified. These patients’ charts were reviewed and information was gleaned for 550 complete patients including gender, height, weight, body mass index, ASA classification, and medical comorbidities. Intra-hospital tests/procedures for these 550 patients and respective costs were obtained from the institution’s financial services department. The tests/procedures for each patient were provided at the CPT code level with associated costs for each test. The CPT codes were broken into six different groups based on Medicare categories: evaluation and management, anesthesia, surgery, radiology, pathology and laboratory, and medicine. Analysis of variance was conducted to explore the association of ASA with the number of hospital tests as well as the costs of these tests.
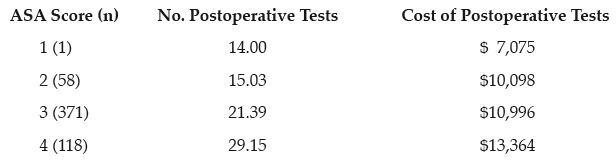
Result: For the 550 patients, there was a significant association between ASA score and number of total hospital tests (P <0.001) and total charges associated with these tests (P = 0.001):
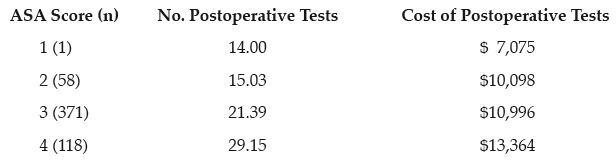
Furthermore, within the six Medicare categories of CPT codes, there were significant associations between ASA score and number of postoperative tests in evaluation and management (P <0.001), surgery (P <0.001), radiology/imaging (P = 0.002), and medicine (P <0.001).
Conclusion: In order to better prepare for payment reform, it is critical to develop a tool that not only allows prediction of LOS, but also offers insight into the resources that will be utilized during a given LOS. Orthopaedic trauma surgeons should consider utilizing the ASA score in thinking about resource management for patients with hip fractures.
• The FDA has not cleared this drug and/or medical device for the use described in this presentation (i.e., the drug or medical device is being discussed for an “off label” use). ◆FDA information not available at time of printing. Δ OTA Grant.