
OTA 2012 Posters
Scientific Poster #14 Hip/Femur OTA-2012
Treatment of Femoral Neck Fractures With a Novel Length-Stable Construct Leads to High Union Rates With Minimal Femoral Neck Shortening
Lionel E. Lazaro, MD; Milton T.M. Little, MD; Marschall B. Berkes, MD;
Patrick C. Schottle, MD; Nadine C. Pardee, BS; David L. Helfet, MD; Dean G. Lorich, MD;Hospital for Special Surgery and Weill Medical College of Cornell University,
New York, New York, USA
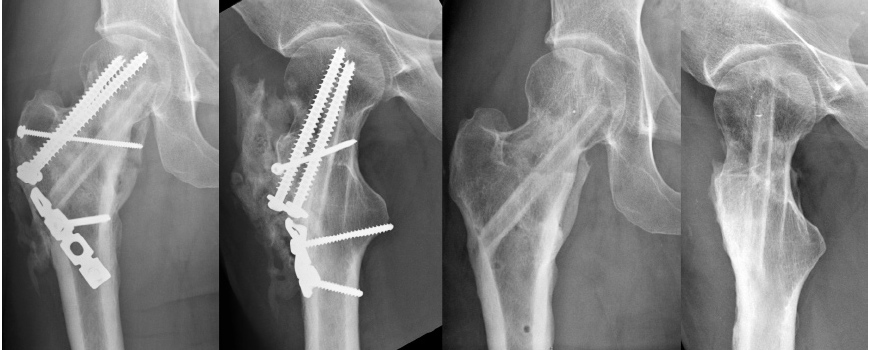
Background/Purpose: The traditional treatment of femoral neck fractures allows sliding in order to permit dynamic compression at the fracture site, but some shortening of the femoral neck invariably follows. Previous studies have demonstrated the negative impact of femoral neck shortening (FNS), but normal hip biomechanics and function are often sacrificed to maximize the potential for fracture healing. Length-stable fixation (open anatomic reduction, intraoperative compression with partially threaded cancellous screws, and final length-stable fixation with fully threaded screws) seemed to provide a solution, with reports of improved clinical outcomes and decreased FNS. Nevertheless, this fixation technique needed refinement to better avoid FNS. We sought to increase the strength of the construct and host bone interface with a strategically placed fibula allograft (control varus/valgus deformity) as a “biologic screw” (figure).

It was our hypothesis that this construct would result in better preservation of intraoperative reduction and improved clinical outcomes compared to historical controls fixed with length stable constructs.
Methods: 18 consecutive femoral neck fractures treated with this novel length-stable construct were initially reviewed. 16 met inclusion criteria with a minimum of 6 months’ radiographic and clinical follow-up. All construct failures were included regardless of length of follow-up. Main outcome measurements included radiographic (reduction maintenance, head migration, FNS, and variation of neck offset and abductor lever arm) and functional (Harris hip score [HHS] and Short Form 36 [SF-36]) outcomes.
Results: Average age was 59.4 years (range, 30-78). The average radiographic and clinical follow-up was 12 months (range, 6-24) and 14.5 months (range, 6-26), respectively. Garden classifications of the fractures included 3 GI, 0 GII, 7 GIII, and 6 GIV (one of which was a revision case after a failed sliding construct; figure).
Anatomic reduction (<5° difference in neck-shaft angle, <2 mm step-off) was achieved in all patients. There was one catastrophic failure (varus displacement with proximal migration of the fibula) 2 weeks after fixation that required total hip replacement. This single failure was attributed to a technical error (misplacement of the fibula allograft) during fixation. The remaining 15 patients achieved bony union. The average displacement of the center of the head did not differ compared to historical controls using length-stable construct (1.65 ± 4.9 mm inferiorly, 0.058 ± 2.9mm medially, 0.6° of increased varus vs historical data of 0.86 mm, 1.23 mm and 0.6°). The average femoral neck collapse was lower compared to historical controls (0.33 ± 2.82 mm vs 1.98 mm; P = 0.049). Average HHS and SF-36 (mental/physical component) did not differ compared to historical control (87 and 49/46 vs 85 and 47/42). The average difference in femoral neck offset and abductor lever arm length did not differ compared to historical controls (0.23 ± 7.1mm and –1.26 ± 6.9mm vs 3.5 ± 8.3mm and 1.5 ± 7.8mm). No subjects demonstrated osteonecrosis on the most recent radiograph (13 patients with >1-year radiographic follow-up). Three patients had removal of hardware, two with excision of extensive heterotopic ossification (Brooker Grade III). Our radiographic outcomes compare favorably with sliding construct fixation data, recently reported as mean 6.2 mm FNS and 4.8 mm inferior shortening.
Conclusion: Intraoperative compression, coupled with this novel length- and angle-stable construct using allograft fibula, can result in high union rates with minimal femoral neck shortening and improved clinical outcomes following femoral neck open reduction and internal fixation.
• The FDA has not cleared this drug and/or medical device for the use described in this presentation (i.e., the drug or medical device is being discussed for an “off label” use). ◆FDA information not available at time of printing. Δ OTA Grant.