OTA 2012 Posters
Scientific Poster #9 Hip/Femur OTA-2012
Assessment of Perfusion to the Femoral Head and Head-Neck Junction Following Surgical Hip Dislocation Using Gadolinium-Enhanced Magnetic Resonance Imaging
Lionel E. Lazaro, MD1; David S. Wellman, MD1; Peter K. Sculco, MD1;
Craig E. Klinger, BS1; Jonathan P. Dyke, PhD2; Nadine C. Pardee, BS1; Edwin P. Su, MD1;
David L. Helfet, MD1; Dean G. Lorich, MD1; 1Hospital for Special Surgery and Weill Medical College of Cornell University,
New York, New York, USA;
2Citigroup Biomedical Imaging Center, Weill Medical College of Cornell University,
New York, New York, USA
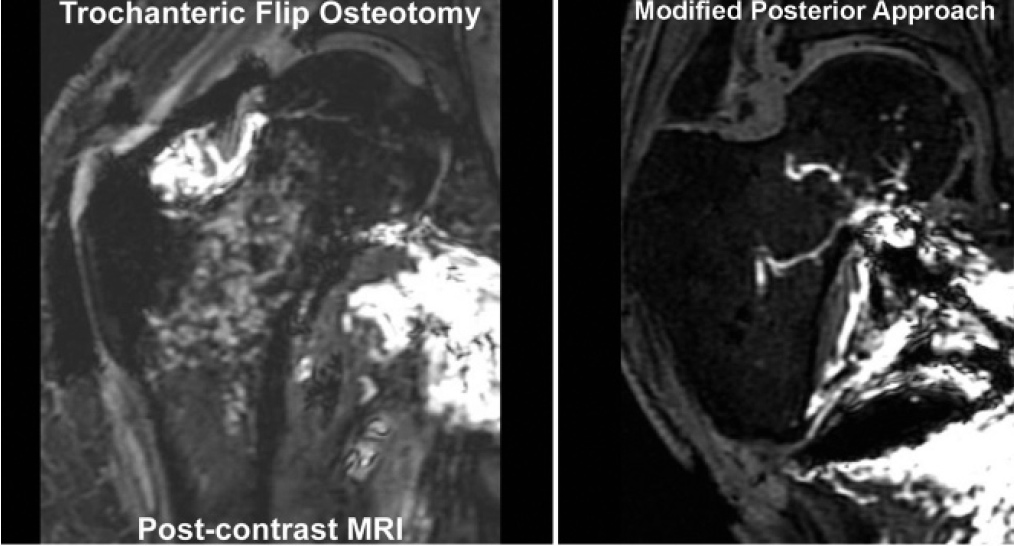
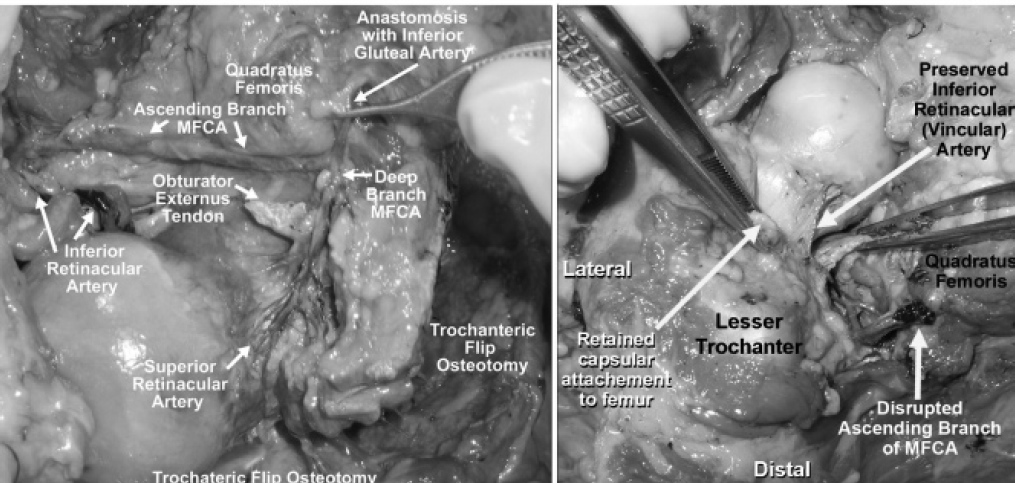
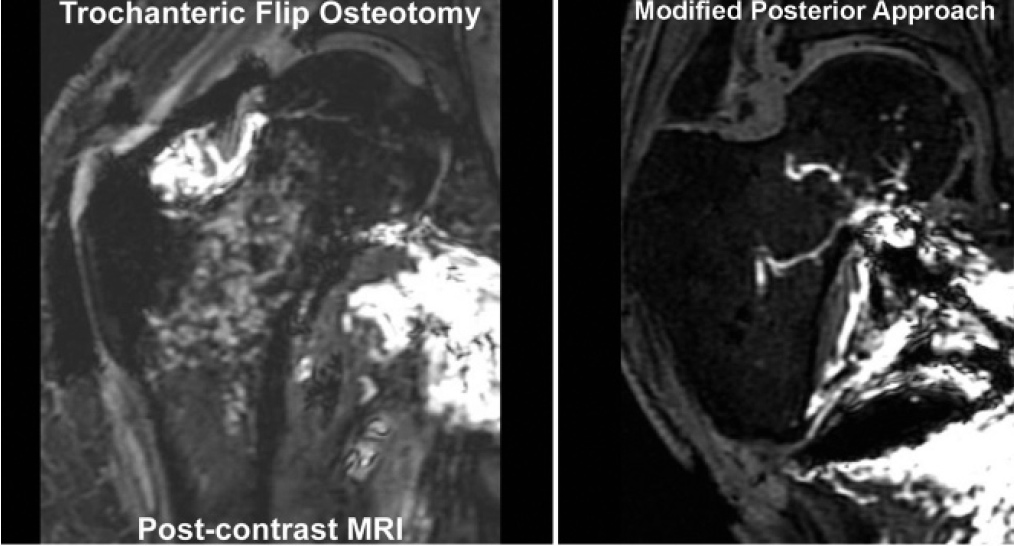
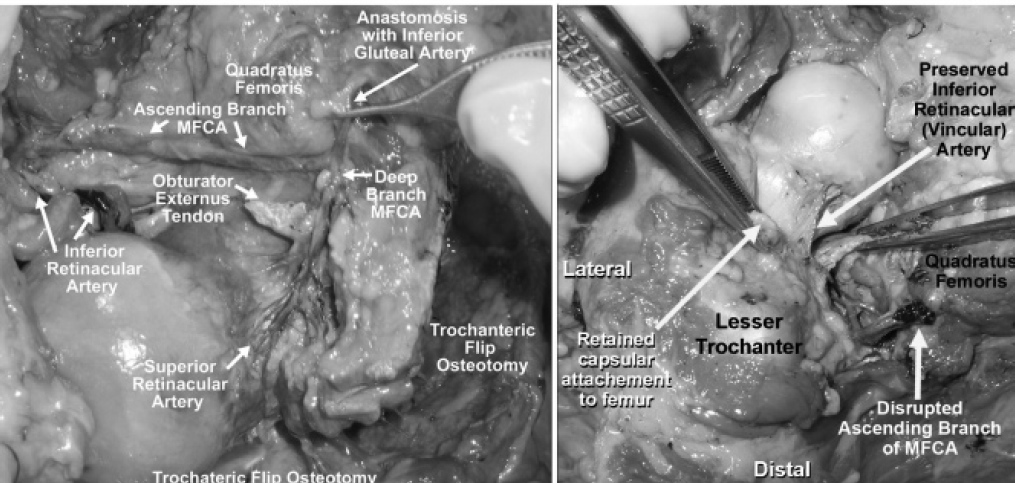
Background/Purpose: Osteonecrosis (ON) of the femoral head (FH) is a significant complication that can arise following surgical hip dislocation. Wide exposure and direct approach to the FH and acetabulum is essential for the treatment of severe hip disease and hip trauma in both the pediatric and adult populations. Ganz et al developed an anterior surgical hip dislocation through a posterior approach using a “trochanteric flip” osteotomy (TFO, upper and lower left figures), which provides excellent exposure while preserving the FH blood supply, as evidenced by intraoperative laser Doppler and the absence of ON on follow-up radiographs. Due to personal preference and comfort, many arthroplasty surgeons continue to use the posterior dislocation approach for resurfacing procedures. During take-down of the external rotator, this approach disrupts the deep and/or ascending branch of medial femoral circumflex artery (MFCA) and the anastomosis with the inferior gluteal artery, compromising the blood supply to the FH. Recently, Steffen et al recommended a “modified blood-preserving posterior approach” (MPA, upper and lower right figures) for hip resurfacing, which employs a capsulotomy at the margin of the acetabulum and was reported to maintain intraoperative FH oxygenation. This study seeks to evaluate and quantify perfusion to the FH and head-neck junction (HNJ) using gadolinium-enhanced MRI following both surgical hip dislocations (TFO and MPA), which has not been previously reported.
Methods: In 40 fresh-frozen cadaveric hips (20 pelvic specimens), we cannulated the MFCA. One hip on each pelvic specimen was randomly chosen to undergo one of two surgical hip dislocations (MPA or TFO), and the contralateral hip was used as a control. Gadolinium was injected through the cannulated MFCA, and pre- and postcontrast MRI was performed. Gadolinium enhancement on the MRI was quantified in both the FH and HNJ for volumetric analysis using custom MRI analysis software. Aurethane compound was then injected and gross dissection was performed to assess the extraosseous vasculature of the FH.
Results: MRI quantification revealed that the TFO group maintained almost full perfusion to the HNJ (98%) and FH (96%). The MPA resulted in a larger reduction of FH and HNJ perfusion with an average perfusion of 48% and 45%, respectively. Gross dissection revealed that 7 of 10 specimens in the MPA group sustained complete disruption of the ascending branch of the MFCA, and no urethane was found in the superior retinacular arterial system. The inferior retinacular artery (vincular artery) was found to be intact with urethane perfusion in 9 of 10 MPA specimens and all the TFO specimens. All specimens in the TFO group had both vessel systems intact, including the superior and inferior retinacular arteries.
Conclusion: This study confirms that the anterior surgical hip dislocation through a TFO preserves the vascular supply to the FH and HNJ, while the MPA results in a marked reduction of the FH and HNJ perfusion, likely secondary to transection of the ascending branch of the MFCA. Despite reduced enhancement, significant perfusion of the FH and HNJ was present in the MPA group, likely due to preservation of the inferior retinacular artery when a careful capsulotomy is performed. Our study provides previously unreported MRI quantitative data on the perfusion to the FH and HNJ following extremely common surgical hip dislocation techniques (TFO, MPA).
• The FDA has not cleared this drug and/or medical device for the use described in this presentation (i.e., the drug or medical device is being discussed for an “off label” use). ◆FDA information not available at time of printing. Δ OTA Grant.